
Cancer
Cancer overview
 Cancer is the biggest cause of death in England and Southampton (GBD 2021). In England, more than 2 million people are currently living with a cancer diagnosis (2022/23) and nearly 140,000 people die from cancer each year (2022). Cancer Research UK predicts that 1 in 2 people will get cancer in England at some point in their lifetime, it is likely to affect all of us in some way. The NHS provide useful information and support to help answer any cancer related questions.
Cancer is the biggest cause of death in England and Southampton (GBD 2021). In England, more than 2 million people are currently living with a cancer diagnosis (2022/23) and nearly 140,000 people die from cancer each year (2022). Cancer Research UK predicts that 1 in 2 people will get cancer in England at some point in their lifetime, it is likely to affect all of us in some way. The NHS provide useful information and support to help answer any cancer related questions.
In 2023, nearly 1 in every 4 deaths in Southampton was from cancer (24.1%). Lung cancer alone caused 1 in every 20 deaths (112 people). As with most public health measures, cancer related statistics and outcomes are worse for people living in more deprived areas. The Office for Health Improvement and Disparities (OHID) produce an inequalities segment tool which shows the relative contribution that nine broad causes of death have on the life expectancy gap between Southampton’s least and most deprived quintiles (2020 to 2021). Females in Southampton’s least deprived quintile live an average of 3.4 years longer than those in the most deprived, 3.5% of this gap is due to cancer. The gap for males is 6 years and nearly one fifth of this gap is because of higher cancer mortality in the most deprived neighbourhoods of Southampton.
What is cancer
Cancer is a condition where the reproduction process of cells in a specific part of the body malfunctions and the cells reproduce uncontrollably. This growth of cancerous cells can invade and destroy surrounding healthy tissue, including organs. The original growth is known as a primary tumour which can spread to other parts of the body causing secondary tumours or “metastases”. Most cancers have four stages, classified by their size and location:
- Stage 1 (early stage): A small, localised tumour which hasn’t spread to other areas of the body or lymph nodes.
- Stage 2 (localised): The cancer has started to affect nearby tissue and lymph nodes.
- Stage 3 (regional spread): The cancer has grown larger and has spread to other areas of the body and distant lymph nodes.
- Stage 4 (distant spread): The cancer has spread to other tissue and organs, sometimes called metastatic or advanced cancer.
There are more than 200 different types of cancer. Breast, lung, prostate and bowel cancer are the most common, making up more than half of all new cancer cases in England. Each cancer has different risk factors, smoking is the biggest cause of lung cancer while high alcohol use is the biggest cause of liver cancer (GBD 2021). Poor diet, high BMI, air pollution, occupational risks (e.g. working with asbestos / toxic fumes) or unprotected exposure to the sun / UV rays can also increase an individual’s risk of getting certain cancers. The risk of developing cancer increases as you get older and some people may be more at risk of developing particular cancers due to their inherited genes.
There is currently no known cure for any type of cancer, however there are treatments that can effectively remove cancer or delay its spread. Many people are successfully treated for cancer, live a full healthy life and die from other causes. Many others are treated for cancer and still die from it, although treatment may give them more years of life. Survivability also varies significantly between different ytpes of cancer. Skin and prostate cancers have a near 100% survival rate (patients surviving the 5 years after their diagnosis), while only 5% of pancreatic cancer patients will survive the 5 years after diagnosis (Cancer Research UK). Cancer survivability has more than doubled in the last 50 years in the UK, this is one of the greatest achievements in medicine and public health. Currently more than half of everyone who is diagnosed with cancer in the UK will survive the next ten years or more (Cancer Research UK).
Cancer screening and early detection
Successful treatment is much more likely if cancer is diagnosed at an earlier stage. Screening can catch cancer in its earliest stages or (in some cases) before it has even formed. Widespread screening and quick referrals can significantly improve cancer outcomes within a population. In England there are 3 major cancer screening programmes:
- Cervical screening (offered to all women aged 25 to 64 to check the health of cells in the cervix. It is offered every 3 years for those aged 25 to 49, and every 5 years from the ages of 50 to 64).
- Breast screening (offered to women aged 50 to 70 to detect early signs of breast cancer. Women over 70 can self-refer).
- Bowel cancer screening (everyone aged 60 to 74 is offered a bowel cancer screening home test kit every 2 years).
Despite the proven efficacy of early cancer diagnosis, cervical and breast cancer screening coverage has been steadily falling in England and Southampton since 2010. In Southampton, 62.3% of eligible women (registered with a GP) have been screened for breast cancer within the last 36 months (2023). This is significantly worse than the England average of 66.2% and is nearly 10 percentage points lower than Southampton’s coverage in 2010 (72.0%). While Southampton and England’s coverage had been steadily decreasing in the years prior to 2020, the COVID-19 pandemic severely disrupted breast cancer screening. England’s coverage has increased year on year since 2021, however Southampton’s recovery has been slower (2023 was actually worse than the year prior).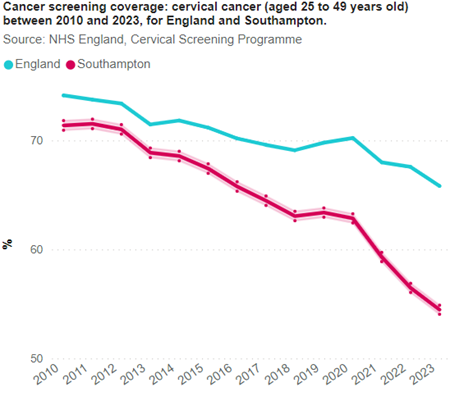 Cervical screening coverage (among people aged 25 to 49 years) in Southampton (54.5% in 2023) is also significantly lower than the England average (65.8%). This is the lowest rate of all our ONS and CIPFA comparators. Only 10 (out of 152) upper tier local authorities in England have a lower rate. Southampton’s coverage was 17 percentage points better in 2011 (71.5%). This decline increased during the COVID-19 pandemic, however cervical screening coverage was not as badly impacted as breast screening.
Cervical screening coverage (among people aged 25 to 49 years) in Southampton (54.5% in 2023) is also significantly lower than the England average (65.8%). This is the lowest rate of all our ONS and CIPFA comparators. Only 10 (out of 152) upper tier local authorities in England have a lower rate. Southampton’s coverage was 17 percentage points better in 2011 (71.5%). This decline increased during the COVID-19 pandemic, however cervical screening coverage was not as badly impacted as breast screening.
While bowel cancer screening coverage is significantly lower in Southampton (68.6%) than the England average (72.0%), it is the cancer screening programme with the best coverage. It was historically the screening programme with the worst coverage for England and Southampton, however coverage has been steadily improving since 2015. This is may be, in part, due to the introduction of less intrusive home testing kits.
Early cancer detection statistics are monitored closely by central government, local government and the NHS as they are such influential public health measures. The NHS has set an ambitious target of diagnosing 75% of all cancers at stage 1 or 2 by 2028. England currently diagnoses 54.4% of all cancers at stage 1 or 2 (in 2021). England’s rate has remained similar since 2013. Southampton was significantly better than England in 2021, achieving 58.8% (and has been improving over time). This is also the best rate compared to all of Southampton’s CIPFA comparator cities. Despite this, Southampton would have needed to diagnose 178 more cancer cases at stage 1 or 2 to achieve the NHS 2028 target of 75%. While this may seem like an unrealistic target, significant technological advances in early detection (particularly in testing and artificial intelligence) are likely to improve early detection rates over the coming years.
Cancer registrations
While cancer treatment and early detection has been getting better, the number of cancer cases has been increasing. More people are getting cancer than ever before in England, cancer prevalence (QOF, all ages) reached 3.5% in 2022/23. This is 2.5 times higher than it was 13 years prior (1.4% in 2009/10). This steady increase in cancer prevalence is a significant cause for concern and can also be seen in Southampton’s cancer registration data (which we have analysed slightly differently to the QOF measure). Southampton’s cancer registrations (directly age standardised cancer registrations per 100,000 people) was 559.3 for the period  2020 - 2024. Southampton's average has been decreasing over time, largely due to falling cancer registrations among males (particularly male colorectal cancer). Female breast cancer registrations have also reduced since 2014 - 2018. Male cancer registrations have historically been significantly higher than female. While both have been reducing, male cancer registrations have fallen at a faster rate. Male and female registrations for all cancers in Southampton were statistically similar in 2020 - 2024 for the first time.
2020 - 2024. Southampton's average has been decreasing over time, largely due to falling cancer registrations among males (particularly male colorectal cancer). Female breast cancer registrations have also reduced since 2014 - 2018. Male cancer registrations have historically been significantly higher than female. While both have been reducing, male cancer registrations have fallen at a faster rate. Male and female registrations for all cancers in Southampton were statistically similar in 2020 - 2024 for the first time.
Lung cancer registrations had historically been significantly higher among men than women in Southampton. Since 2014 – 2018, male registrations per 100,000 DSR have been improving year on year while female rates have remained similar. This gender gap almost completely closed in 2018 – 2022, as the male DSR rate (98.7 per 100,000) was 6.7 per 100,000 higher than the female rate (92.0 per 100,000).
For the period 2020 - 2024, the west of the city had a significantly higher cancer registrations for all cancers (525.5 per 100,000 DSR), this was mostly caused by significantly higher female breast cancer registrations than the rest of the city.
Across England cancer registrations have been increasing. The reasons behind the steady growth in cancer rates is unknown, however increases in obesity and the consumption of processed foods have been cited as potential causes, particularly for the increase in colorectal cancers. Other potential reasons may be that we are simply living longer (and age is one of the biggest risk factors for cancer) or the fact that more cancer cases are now being detected as screening and diagnosis techniques improve. The fact that cancer cases are increasing while cancer mortality is decreasing suggests better diagnosis may be a major factor.
Cancer services
Fast cancer referrals, diagnoses and treatment are proven to improve cancer outcomes. Having confirmed or suspected cancer is stressful in its self, longer wait times can cause additional stress to patients. GPs, dentists, optometrists (eye doctors) or nurses can arrange referrals for a patient to see a specialist, or to have further tests. An urgent referral can be worrying, but more than 9 in every 10 people referred this way will not have a diagnosis of cancer. Wait times have been getting worse across England over the last 10 years, however University Hospital Southampton NHS Trust (UHS) has some of the best referral wait time statistics in the country. NHS England has introduced a new target called the Faster Diagnosis Standard (FDS). The target is that you should not wait more than 28 days from referral to finding out whether you have cancer or not. The FDS applies to anyone with a suspected cancer, even if you have been treated for cancer in the past. The FDS is part of a wider NHS England plan to focus more on the speed that someone gets their results and diagnosis. It applies to those people who are referred:
- By their GP for suspected cancer.
- By their GP with breast symptoms where cancer is not suspected.
- Following an abnormal screening result from a cancer screening test.
In 2023, UHS achieved the FDS target for 80.2% of patients. This is significantly higher than the operational standard of 75% and the England average of 72.0%. Despite this relatively good performance, this still equates to more than 5,000 UHS patients waiting longer than 28 days to find out if they have cancer or not in 2023.
There are also waiting time targets for cancer treatment. In England, Scotland and Northern Ireland the current targets are:
- No more than 2 months (62 days) wait between the date the hospital receives an urgent suspected cancer referral and the start of treatment.
- No more than 31 days wait between the meeting at which the patient and doctor agree the treatment plan and the start of treatment.
UHS achieved the 62 day target for 69.2% of patients in 2023, significantly worse than the operational standard of 85% but significantly better than the England average of 64.2%. UHS is performing significantly better on this measure for the first 5 months of 2024, currently averaging at 77.0%.
However, UHS is performing worse than the England average for the 31 day target. In 2023 it achiceved this target for 83.9% of patients, the England average was 90.1%. Both were significantly worse than the operational standard of 96%. This indicator is also looking better for UHS in the first 5 months of 2024, currently achieving 89.5%.
Cancer mortality
 In 2023, nearly 1 in every 4 deaths in Southampton was from cancer (24.1%). Lung cancer alone caused 1 in every 20 deaths (112 people). Southampton has worse cancer mortality than England for almost all mortality measures. Despite cancer mortality decreasing and getting better for England and Southampton since 2001 – 2003, Southampton’s mortality has always been slightly higher than the England average. The reduction in cancer mortality has been slower in Southampton than the rest of England, causing the gap between England and Southampton to grow. For the period 2020 – 2022, cancer mortality in Southampton (278.5 DSR per 100,000) was significantly higher than the England average (251.7 DSR per 100,000).
In 2023, nearly 1 in every 4 deaths in Southampton was from cancer (24.1%). Lung cancer alone caused 1 in every 20 deaths (112 people). Southampton has worse cancer mortality than England for almost all mortality measures. Despite cancer mortality decreasing and getting better for England and Southampton since 2001 – 2003, Southampton’s mortality has always been slightly higher than the England average. The reduction in cancer mortality has been slower in Southampton than the rest of England, causing the gap between England and Southampton to grow. For the period 2020 – 2022, cancer mortality in Southampton (278.5 DSR per 100,000) was significantly higher than the England average (251.7 DSR per 100,000).
For the period 2020 – 2022, Southampton had the 10th highest rate in England for colorectal cancer mortality (32.2 DSR per 100,000), significantly higher than the England average of 25.7. Southampton’s cancer mortality is also worse than the England average for lung, bladder, oesophageal, alcohol related cancer, ‘preventable’ cancer and under 75 cancer mortality.
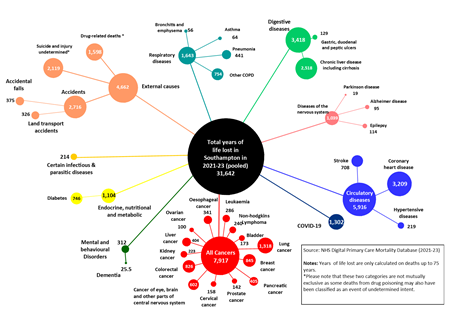 Years of life lost (YLL) is a measure of the average time a person would have lived had they not died before the age of 75 years. This data helps measure the social and economic loss from dying younger and highlights the specific causes of death affecting younger people. In 2023, nearly 11,000 years of life were lost for Southampton residents aged under 75 years. During this period cancer was by far the biggest cause of life lost, responsible for 25.5% of YLL (the equivalent of 2,767 years). Lung, breast and colorectal cancer caused the most YLL of all the cancers. Colorectal cancer caused only 1.8% of all cancer deaths but accounted for 7.9% of YLL, reflecting the younger average age of people who died from colorectal cancer in Southampton. Conversely, prostate cancer caused 1.4% of all cancer deaths but only accounted for 0.7% of YLL.
Years of life lost (YLL) is a measure of the average time a person would have lived had they not died before the age of 75 years. This data helps measure the social and economic loss from dying younger and highlights the specific causes of death affecting younger people. In 2023, nearly 11,000 years of life were lost for Southampton residents aged under 75 years. During this period cancer was by far the biggest cause of life lost, responsible for 25.5% of YLL (the equivalent of 2,767 years). Lung, breast and colorectal cancer caused the most YLL of all the cancers. Colorectal cancer caused only 1.8% of all cancer deaths but accounted for 7.9% of YLL, reflecting the younger average age of people who died from colorectal cancer in Southampton. Conversely, prostate cancer caused 1.4% of all cancer deaths but only accounted for 0.7% of YLL.
Resources
NHS cancer
Information on spotting cancer, reducing risk, wait times, cancer services and more information on each type of cancer.
Mortality bubble charts
Below are two bubble charts showing all cause mortality and the number of years of life lost. In these charts the size of the bubble is proportionate to the number of deaths and years of life lost.
IHME – Global Burden of Disease (GBD)
The Global Burden of Disease (GBD) study provides a comprehensive picture of mortality and disability across countries, time, age, and sex. It quantifies health loss from hundreds of diseases, injuries, and risk factors, so that health systems can be improved and disparities eliminated.
Smoking dashboard
Smoking is the leading cause of preventable death and disease in the UK and the leading factor for disability-adjusted life years. Every year around 78,000 people in the UK, die from smoking, with many more living with debilitating smoking-related illnesses. Smoking increases the risk of developing more than 50 serious health conditions. In addition, one in ten pregnant women still smoke nationally with the associated risks of miscarriage, premature birth, still birth, low birth weight and neonatal complications. This dashboard presents a wide range of data regarding smoking, to provide intelligence to help drive strategic decision making, such a the Southampton Tobacco, Alcohol and Drugs Strategy.
Tobacco, Alcohol and Drugs Strategy 2023 - 2028
This strategy describes our vision for how we, as a council, will reduce the harm to people who use tobacco, alcohol and drugs, as well as harm to people around them, and harm across the city of Southampton as a whole.
Tobacco, Alcohol and Drugs Strategy (TAD) dashboard
The TAD dashboard presents a range of data to help measure how well we, as a council, will reduce the harm to people who use tobacco, alcohol and drugs, as well as harm to people around them, and harm across the city of Southampton as a whole. This will be monitored through the Tobacco, Alcohol and Drugs Strategy 2023-2028.
ONS - Adult smoking habits in the UK: 2022
Cigarette smoking habits among adults in the UK, including the proportion of people who smoke, demographic breakdowns, changes over time and use of e-cigarettes.
NHS England - Statistics on Public Health
This publication series presents or signposts to a range of information relating to a range of Public Health Statistics on Alcohol, Drug use, Obesity, Physical Activity, Diet and Smoking.
Alcohol dashboard
This dashboard shows key alcohol related data for Southampton, England and other comparator cities. Data in this dashboard has been compiled from a range of publicly available sources including the Office for Health Improvement and Disparities (OHID).
Life expectancy and mortality dashboard
The life expectancy and mortality dashboard present a range of data regarding life expectancy and mortality, to provide intelligence to help drive strategic decision making. Analysis includes benchmarking against statistical neighbours and trends over time for all indicators included. Some indicators include analysis at sub-city levels, by Southampton wards, primary care networks (PCNs) and deprivation quintiles.
Hampshire Major Conditions Report
Analysis of GP level long term / major health conditions in Hampshire, provided by Hampshire County Council.
Last updated: 04 December 2024