
Mental health
 Mental health background
Mental health background
One in four adults and one in 10 children experience mental illness at any one time, and many more of us know and maybe also care for people experiencing mental illness. Improved mental health and wellbeing is associated with a range of better outcomes for people of all ages and backgrounds (NHS England mental health information).
Partners from across Southampton came together to develop a Mental Health and Wellbeing Strategy. The shared vision is that people in Southampton have good mental health and wellbeing, whatever their background or the circumstances in which they live. It focuses on preventing poor mental health and promoting wellbeing, looking at all the things that are important for mental health and wellbeing. The strategy outlines the six priority areas for action:
- There is a positive culture that promotes mental health and wellbeing in Southampton
- Having a greater focus on the areas of people’s lives that impact their mental health
- People in Southampton get support for their mental health and wellbeing when needed
- People have the opportunity to have positive mental health and wellbeing and are able to benefit from support that is right for them
- Children and young people get the best start in life for their mental health and wellbeing and families are supported
- Working together to prevent suicide and self-harm, and support those who are impacted
Southampton City Council and Hampshire and Isle of Wight Integrated Care Partnership (ICP) through the Health and Wellbeing Board are committed to working together with the people of Southampton to improve the health and wellbeing of residents, with an equal focus on physical and mental health. The ICP have produced an Integrated Care Strategy for Hampshire and Isle of Wight, which includes mental wellbeing as one of the five key areas of focus. The priorities within this area are to:
- Better connect people to avoid loneliness and social isolation
- Promote emotional wellbeing and prevent psychological harm
- Improve mental health and emotional resilience for children and young people
- Focused work on suicide prevention
- Improve access to bereavement support
- Address inequalities in access and services
- Support mental health and wellbeing of staff
It is important to make sure the city is a healthy place by ensuring services are delivered as efficiently as possible, targeting them towards those people who need them most. The Southampton Health and Wellbeing Strategy (2017-25) recognises that it is particularly important to increase access to appropriate mental health services as early as possible and when they are needed; prioritising and promoting mental health and wellbeing as being equally important as physical health.
More information can be found in the mental health dashboard below and the resources section at the end of the page.
Who is at risk and why?
The risk factors that are linked to poor mental health can include, housing, educational attainment, deprivation, physical health and preparation for employment. Some examples from other pages on the Southampton Data Observatory include:
- Deprivation– Mental health problems are unevenly distributed across society with disproportionate impacts on different groups such as people living in poverty. The 2019 Index of Multiple Deprivation ranks Southampton 55th (where 1 is the most deprived) out of 317 local authorities. Southampton has 19 neighbourhoods, out of 148 (Lower Super Output Areas -LSOA 2011) within the 10% most deprived in England and one in the 10% least deprived. Southampton has 45.9% of its population living in the most deprived 30% neighbourhoods in England, people living in poverty are more at risk of poorer mental health. More information can be found on the Health inequalities and Deprivation and poverty pages.
- Physical health – poor physical health, disability and those with long-term conditions are risk factors for poor mental health. Those with existing long-term conditions such as asthma, diabetes or arthritis are 2 to 3 times more likely to develop a mental illness. In Southampton, in 2023/24, 18.762 (6.0%) registered patients, aged 6 and over, have an active diagnosis of asthma. In 2023/24, 17,450 (6.4%) people aged 17 and over have diabetes. GP practice data shows 10.8% of the registered population are living with 3 or more long-term conditions. More information can be found on the Health conditions page.
- Loneliness and lack of social interaction – both can occur at any time in an individual’s life, the circumstances that increase the risk of loneliness vary with age. For example, leaving education can be a vulnerable time for younger people, whereas the death of a loved one or the onset of an illness can often be a time of vulnerability for older people. In the 2020 City Survey, the majority of people (67%) feel a low level of loneliness and isolation in their daily life. During the pandemic 1 in 4 respondents reported high levels of loneliness. The demographic breakdowns show that younger age groups are more likely to report being lonely, male respondents feel less lonely than female respondents. Levels of loneliness and social isolation show an increase of five percentage points between 2018 and 2020 (16% scored 7-10 in 2020). More information can be found in the Research section and Social isolation page.
- Housing - the quality of housing is crucial to health and wellbeing, especially for the vulnerable, young and old can be particularly susceptible to poor health associated with inadequate heating and insulation, damp and overcrowding. Poor housing conditions can contribute to a range of physical and mental illnesses and children growing up in difficult housing conditions are more likely to suffer severe ill-health and disability during childhood and or early adulthood. More information is available on the Housing and homelessness page.
- Individual characteristics – such as resilience and the availability of ‘social capital’, which are the social networks and relationships an individual can access in times of difficulty, which in some circumstances can positively influence health outcomes.
- Inequalities in mental health and wellbeing can be identified in various population groups:
Ethnic groups: People from some ethnic groups can have higher rates of diagnosis of mental illness, and may cause delays in support, hospital admissions due to mental illness, poor treatment outcomes and disengagement from mental health services. The 2021 Census recorded 79,440 people in the city who do not consider themselves white British and there are 48,090 people who do not consider themselves to have a white ethnicity. Of these 79,440 people 39.8% of non-white British residents and 45.8% of non-white residents are under the age of 25 years. More information is available on Ethnicity, language and identity page.
Looked after children in care and care leavers: In England, half of looked after children meet the criteria for a mental health disorder. On 31 March 2023, Southampton had 538 children looked after. In 2022/23, 43.0% of children looked after were identified whose emotional wellbeing was cause for concern, higher but not significantly than the England average of 40.0%.
People who identify as lesbian, gay, bisexual, trans, queer, questioning and asexual (known as LGBTQ+): In England, half of LGBTQ+ people experience depression, three in five experience anxiety, one in eight LGBTQ+ people (aged 18 to 24) had attempted to end their life and almost half of trans people had thought about taking their life. Of the people who answered the Census 2021 question on sexual orientation, 10,082 identified as gay, lesbian, or other non-heterosexual orientations including pansexual, asexual and queer. For more detailed breakdowns for these groups see the 2021 Census page.
Carers: Carers are twice as likely to have a long-term physical or mental health condition. Only 30% of adult carers in Southampton get as much social contact as they would like. In the 2021 Census 18,136 people (7.7% of the population) said they provide some level of unpaid care in Southampton. More information on carers is available on the Carers page.
Young carers: Nationally, 60% young carers feel their caring role has affected their emotional wellbeing. Their caring role can be associated with stress, anxiety, low self-esteem, missing school, not participating in activities, and a lack of social connections. The 2021 Census recorded in Southampton 314 unpaid carers are under 16, of which, 103 (a third) provide more than 20 hours of care a week. This is likely to be an underestimate. More information on carers is available on the Carers page.
Neurodiversity: 1 in 7 people (15%) in the UK are neurodivergent and evidence shows that neurodivergent people have a higher risk of poorer mental health and suicide. An estimated 70% of people who are on the autistic spectrum have a co-occurring mental health condition. Out of Southampton’s population this is estimated to be 39,600 people.
Co-occurring conditions: Nearly two thirds of people entering drug and alcohol treatment programmes have mental health needs. People with a musculoskeletal condition in Southampton are 1.9 times more likely to also have a mental health condition compared to those who don’t. This is higher than the ratio for England of 1.4 times.
Social care users: Half of all adult social care users in Southampton have depression or anxiety.
Homeless households and rough sleepers: In Southampton 10.4 per 1,000 households are assessed as being homeless. 45% of people experiencing homelessness have been diagnosed with a mental health issue. This rises to 8 out of 10 people who are sleeping rough.
More information can be found in the mental health dashboard below and the resources section at the end of the page.
Children and young people
The Southampton City Children and Young People's Emotional and Mental Health Wellbeing Plan: 2021 - 2024 sets out the vision for the importance of partnership working; social and emotional mental health becomes 'everyone's business' across Southampton. The plan sets out the vision for Southampton’s children and young people to have the best start in life and enjoy positive emotional wellbeing and mental health, which will be achieved by:
- Supporting professionals working with children and young people to have a shared understanding of positive emotional wellbeing and mental health in their work
- Ensuring that children and young people have access to a range of early interventions to support their emotional wellbeing and mental health needs which will prevent difficulties escalating and some may require specialist mental health services
- Ensuring a clear needs-led model of support for children and young people which will provide access to the right help at the right time through all stages of their emotional and mental health development
- Improve equalities in access, experience and outcomes for groups faring worse than others or more at risk of poor mental health
Children with mental, emotional or social needs are identified in schools where an education health care plan, statement or other support is put in place to help children and young people reach their potential. In 2022/23, 4.0% of primary, secondary and special school Southampton pupils were categorised with Special Education Needs (SEN) where the primary needs are social, emotional and mental health (significantly higher than 3.3% in England).
More information and indicators relating to children and young people’s mental health can be found in the mental health dashboard below and in the resources section at the bottom of the page.
Mental health conditions
Mental health conditions, refer to a wide range of mental health diagnosis, these conditions can alter mood, thinking and behaviour. The most frequently occurring include common mental disorders, depression, severe mental illnesses, including Schizophrenia and bipolar disorder and self-reported wellbeing, more details are available below.
Common mental disorders (CMD)
In 2017, it was estimated that 18.7% of the Southampton population were likely to have a common mental health disorder, (significantly higher than the estimate for England of 16.9%). These estimates do not take into consideration those people living in institutional settings or those people experiencing homelessness.
In the same period, it is estimated that 11.5% of people aged 65 and over have a common mental disorder, higher but not significantly from the England average of 10.2%.
Depression
Depression affects different people in different ways it can include some or all of the following symptoms: feelings of sadness and hopelessness; losing interest in things; feeling tearful; feeling constantly tired, sleeping badly, having no appetite. It can result in significantly reduced the quality of life for patients, their family and carers (NHS depression).
In 2022/23, 32,971 patients or 12.8% of Southampton registered patients aged 18 and over, have depression this is lower than the England average of 13.2%.
For newly diagnoses in 2023/24, 4,009 or 1.5% of Southampton registered patients aged 18, were newly diagnosed as having depression. The same as the England average.
Severe mental illnesses
Severe mental illness (SMI) refers to people with psychological problems that are often so debilitating that their ability to engage in functional and occupational activities is severely impaired. Schizophrenia and bipolar disorder are often referred to as an SMI.
In 2023/24, 3,434 or 1.03% of Southampton patients with schizophrenia, bipolar affective disorder and other psychoses as recorded on practice disease registers, similar to the England average of 0.96%.
Self-reported wellbeing
People who have a higher wellbeing tend to have lower rates of illness and recover more quickly and for longer and generally have better physical and mental health. Mental health illnesses may be impacted by a low happiness score.
In 2022/23, ONS found, that when asked “Overall, how happy did you feel yesterday?” 13.1% of people surveyed aged (16 and over), in Southampton had a low happiness score, higher than the England average of 8.9%.
From the same survey respondents were asked about their anxiety, "Overall, how anxious did you feel yesterday?" for respondents from Southampton 33.8% had a high anxiety score (significantly higher when compared to the England average of 23.3%).
Another question asked "Overall, to what extent do you feel the things you do in your life are worthwhile?" of those surveyed in Southampton 4.2% reported that they had a low worthwhile score (lower but not significantly that the England average of 4.4%).
More information can be found in the mental health dashboard below and the resources section at the end of the page.
Self-harm
The Southampton Suicide prevention plan (2020-2023) includes information on self-harm. Self-harm is a concern in its own right, as well as being a risk factor in suicide. Not everyone that self-harms will have suicidal thoughts, whilst not everyone that dies by suicide will have self-harmed. Of the 38 deaths by suicide in 2017 and 2018 that were audited and 23% were known to have a history of self-harm. The local audit of Coroner’s records will under-estimate the individuals that have self-harmed as it is well documented that many people who self-harm do not seek help from health or other services and so self-harm episodes are not recoded.
It is hard to find the real prevalence of self-harm in the population as much of it is hidden, but one of the measures available is emergency hospital admissions for intentional self-harm. In 2023/24, there were 725 emergency admissions a rate of 261.7 DSR per 100,000, although this rate is falling it is still significantly higher than the England average of 117.0 DSR per 100,000. The hospital admissions rate as a result of self-harm for 10 to 24 year olds in 2023/24 was 484.7 DSR per 100,000 population, significantly higher than the England average of 266.6 per 100,000 population. National risk factors for self-harm include the following:
- Women - rates are two to three times higher in women than men
- Young people - 10% to 13% of 15 to 16 year olds have self-harmed in their lifetime
- Mental health disorders including depression and anxiety
- People who have or are recovering from drug and alcohol problems
- People who are lesbian, gay, bisexual or gender reassigned
- Socially deprived people living in urban areas
- Women of black and South-Asian ethnicity
- Groups including veterans, prisoners, those with learning disabilities, and those in care settings
- Individual elements including personality traits, family experiences (being single, divorced or
- living alone), exposure to trauma (including bullying, abuse or adverse childhood experiences),
- life events, cultural beliefs, social isolation and income.
More information can be found in the mental health dashboard below and the resources section at the end of the page.
Dementia
In 2024, it is estimated that 1,853 (66.8%) of Southampton registered patients, aged over 65 years have been recorded with a diagnosis of dementia (similar to the England average of 64.8%).
Dementia is more common in those aged over 65 years but can affect people as young as in their 30s. It is estimated that in Southampton 2.18 crude rate per 10,000 registered population were recorded to have dementia aged under 65 years old, lower than the England average of 3.05 per 10,000.
The prevalence of dementia in those aged over 65 is expected to rise. Estimates from Projecting Older People Population Information (POPPI), suggest that the number of people with dementia aged over 65 years could rise by 36.8% between 2023 and 2040, lower when compared with 45.6% in England.
However, the expected rise in prevalence may not be directly related to an increase in prevalence, it could be a combination of a number of factors; for instance, GPs are becoming better at diagnosing and recording dementia, which is likely to continue to improve (NHS England).
More information can be found in the mental health dashboard below and the resources section at the end of the page.
Suicide prevention
Suicide is a significant cause of death in young adults and a leading cause of years of life lost. The Southampton Suicide prevention plan (2020-2023) aims to reduce the number of suicides in Southampton, and ensure provision of support to those bereaved by suicide, focusing on but not limited to groups at high risk of taking their own life. The priorities for this plan are:
- Achieve city wide leadership for suicide prevention
- Reduce the risk of suicide in key high-risk groups
- Tailor approaches to improve mental health in specific groups
- Reduce access to the means of suicide
- Provide better information and support to those bereaved or affected by suicide
- Support the media in delivering sensitive approaches to suicide and suicidal behaviours.
- Support research, data collection and monitoring
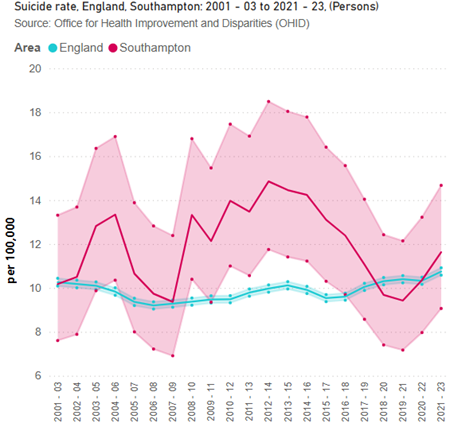 In Southampton, the suicide rate has fallen in recent years from 14.9 deaths per 100,000 in 2012-14 to 11.6 in 2021-23. Southampton has a similar rate to England (10.7 deaths per 100,000) and higher than the South East (10.4 deaths per 100,000) average.
In Southampton, the suicide rate has fallen in recent years from 14.9 deaths per 100,000 in 2012-14 to 11.6 in 2021-23. Southampton has a similar rate to England (10.7 deaths per 100,000) and higher than the South East (10.4 deaths per 100,000) average.
Southampton’s suicide rate is the 9th lowest when compared to 15 similar Local Authorities (using the CIPFA nearest neighbour definition). Translated into numbers of registered deaths by suicide, we know that about 25 residents in Southampton take their own life by suicide each year (based on 2021-23 data).
Southampton City Council Public Health works with the coroner’s office to undertake suicide audits to gather intelligence on deaths by suicide. Of the deaths by suicide between January 2019 and December 2020 (2019-2020 Suicide Audit):
- 74% were male 26% were female
- The average age overall for males and females was 45 years
- For males the average age was 47 years and 39 years for females
- The age bands with the highest prevalence in males were 25 to 39 years and 50 to 59 years
- The ethnic breakdown:
- 67% were white British
- 13% white other
- 6% Black (African, Caribbean or Black British)
- 4% Asian or Asian British
- 2% Mixed or Multiple Ethnicity
- 9% are not known
- 24% were in contact with mental health services at the time of death, a further 22% had been in contact previously. 26% had been in contact with their GP in the 2 weeks preceding their death
- 56% were known to have a history of suicide attempts or self-harm
- 59% of those who died were employed or self-employed, 15% unemployed, 9% retired, 4% students, 4% long term sick or disabled, 9% not known or other
- The most common adverse life experiences recorded include mental illness, relationship problems, traumatic childhood, bereaved or affected by suicide, physical illness, bereavement, contact with the criminal justice system, drug use or addiction, financial difficulties, pain management, and work related stress
In 2021-23, the suicide rate for males in Southampton was 16.7 DSR per 100,000 population aged 10 and over, similar to the England average of 16.4. Compared to 6.7 DSR per 100,000 aged 10 and over for females, similar to the England average of 5.4 DSR.
Looking at the years of life lost due to suicide, in Southampton for 2020-22, is 34.7 per DSR for people aged 15-74 years per 10,000 population (3 year average) similar when compared to the England average of 34.1 DSR per 10,000 population for the same population base.
For males the rate was 49.1 DSR per 10,000 population compared to a rate of 20.0 DSR per 10,000 population for females in Southampton. This compares to the England rate of 51.5 DSR per 10,000 population for males and 17.2 DSR per 10,000 population for females. Both Southampton figures are similar to England.
More information can be found in the mental health dashboard below and the resources section at the end of the page.
People with learning disabilities
People with a learning disability often have a significantly higher prevalence of other health conditions compared to people without learning disabilities. There are many reasons why people with a learning disability are more likely to experience poor mental health. These include biology and genetics, higher incidence of negative life events, access to resources and coping skills. In the Hampshire, Isle of Wight and Southampton area, this includes:
- Dementia – 1.5% of patients with a learning disability have a diagnosis of dementia higher when compared to 0.8% of patients without a learning disability
- Depression - 15.2% of patients with a learning disability have and active diagnosis of depression, slightly lower when compared to patients without a learning disability (15.9%)
- Severe mental illness – 6.5% of patients with a learning disability have a diagnosis of severe mental illness significantly higher than those patients without a learning disability (0.8%)
More information on people with Learning Disabilities can be found on the Learning Disabilities page.
Resources
Mental health dashboard
The mental health dashboard presents a range of data related to mental health. Data in this dashboard is compiled from a range of publicly available sources, accessed through data tools from the Office for Health Improvement & Disparities (OHID).
Mental Health and Wellbeing Strategy
The strategy focuses on preventing poor mental health and promoting wellbeing, looking at all the things that are important for mental health and wellbeing.
Health and Wellbeing Strategy 2017-2025
Our vision is that Southampton has a culture and environment that promotes and supports health and wellbeing for all. Our ambition is to significantly improve health and wellbeing outcomes and reduce citywide health inequalities in Southampton by 2025.
Southampton suicide prevention plan (2020-2023)
The suicide prevention plan aims to reduce the number of suicides in Southampton and ensure provision of support to those bereaved by suicide, focusing on but not limited to groups at high risk of taking their own life.
OHID – Public mental health dashboard
The dashboard is divided into sections relating to the requirements of a JSNA, containing pages where both narrative and data are presented. Indicators are taken from Office for Health Improvement and Disparities (OHID) Fingertips.
OHID – Fingertips – Mental health tools
These system profiling tools are available to all. They are primarily intended to provide better access to information and intelligence to support commissioning, planning and providing services locally. The tools bring together a wide range of publicly available information to offer a broad picture of mental health and dementia and provide the means to focus on specific topic areas. The tools enable and advocate benchmarking against peers. The core aim is to provide information for improvement, not judgement.
NHS England – Mental Health Services Monthly Statistics
This publication provides the timeliest picture available of people using NHS funded secondary mental health, learning disabilities and autism services in England.
Hampshire and Isle of Wight – Integrated Care Strategy
Southampton City Council and Hampshire and Isle of Wight Integrated Care Partnership (ICP) through the Health and Wellbeing Board are committed to working together with the people of Southampton to improve the health and wellbeing of residents, with an equal focus on physical and mental health.
NHS England - Mental Health of Children and Young People in England, 2020: Wave 1 follow up to the 2017 survey
This is the first in a series of follow up reports to the Mental Health and Young People Survey (MHCYP) 2017, exploring the mental health of children and young people in July 2020, during the Coronavirus (COVID-19) pandemic and changes since 2017. Experiences of family life, education and services, and worries and anxieties during the COVID-19 pandemic are also examined.
Oxford Brookes University - Projecting Older People Population Information System (POPPI)
This view-only system is developed by the Institute of Public Care (IPC). It is for use by local authority planners and commissioners of social care provision in England, together with providers. It is a programme designed to help explore the possible impact that demography and certain conditions may have on populations aged 65 and over.
Public First - The Other Pandemic: The Impact of Covid-19 on Britain’s Mental Health
In February 2021, a survey was carried out by Public First about people’s mental health during the pandemic. The survey results concluded that 40% of respondents said their mental health has been negatively affected in the last 12 months. The report shows that Coronavirus has taken on mental health in all parts of society – but especially women, the less well-off and young people.
Last updated: 17 March 2025